September 3, 2024
The Mental Impact Of Desire Urinary Incontinence
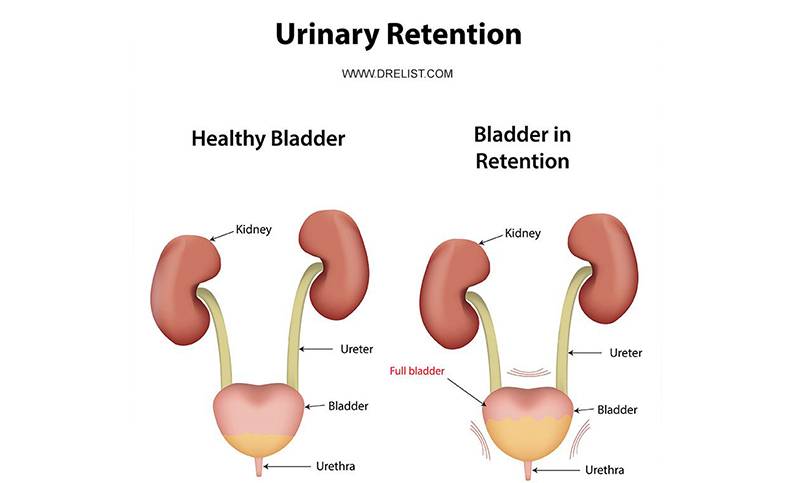
Dealing With Urinary Incontinence: Social And Emotional Difficulties One of the key mental results of urinary system incontinence is the feeling of embarrassment and shame that many individuals experience. The anxiety of leakages and mishaps can bring about social withdrawal, avoidance of social activities, and sensations of isolation. This can produce a vicious circle where individuals end up being significantly separated, resulting in additional decreases in psychological wellness. The history needs to be made use of to determine the kind, severity, concern, and period of urinary system incontinence. Invalidating diaries may help provide information concerning episodes of urinary incontinence.- Overflow urinary incontinence is the uncontrolled leak of pee from an overdistended bladder as a result of damaged detrusor contractility and bladder outlet obstruction.
- The research study data was accumulated on the internet in between March and October 2020 utilizing the online survey platform Google Forms (consisting of all the product explained over).
- There are several points you can do, and items you can utilize, to make urinary incontinence less of a problem to cope with in your life as a whole, as well as at the workplace.
- Alternatively, significant modifications might occur, including a need to utilize self-catheterization for a long term postoperative period.
The Value Of Penile Implants In Enhancing Quality Of Life *
Prompt incontinence occurs when the muscle mass of the bladder-- the body organ that shops urine-- contracts involuntarily, triggering an abrupt and solid urge to pee even when the bladder isn't complete. This can be very disruptive as it causes regular washroom sees, considerably affecting a person's everyday activities and general lifestyle. Having solid pelvic floor muscles and an understanding of which muscle mass to press can enhance digestive tract control. If you have impulse urinary incontinence and other therapies have not benefited you, shots of botulinum contaminant (Botox) may Menopause-Related Incontinence be an option. Your urologist infuses it into your bladder to help relax the muscles there. This gives you more time to reach the bathroom when you really feel the urge to pee.According To The Intensity Of Urine Loss
How to manage urinary incontinence?
- " Easing urinary system incontinence begins with understanding which kind of urinary incontinence you're experiencing and
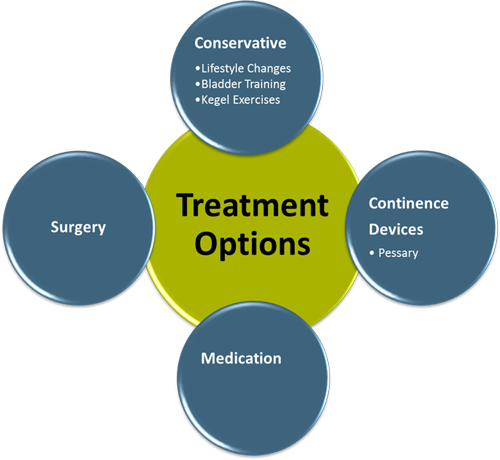
- what's creating it," states Dr. Workout your pelvic floor.Take supplements.Do yoga exercise to relax.Make way of living changes.Consciously beverage water.Seek medical treatment.Consider behavioural therapy.Find your neighborhood. Administration and therapy for urinary incontinence Options may consist of: raised fluid intake of as much as 2 litres a day. high-fibre diet. pelvic floor workouts. The eCoin system, accepted by the united state Food and Drug Administration "in March 2022 for the therapy of necessity urinary incontinence, is based on tibial nerve'stimulation. The tibial nerve is involved in movement and feeling

Social Links